Your doctor may recommend surgery if you suffer a serious neck injury at work. The decision about whether you need neck surgery and which type of surgery would be best for you should be made by you and your doctor.
Doctors perform many different types of neck surgery to relieve pain and impairment that comes from work injuries. Some of the most common types of neck surgeries performed in workers compensation cases include the following:
- Cervical discectomies,
- Cervical fusions, and
- Cervical laminectomies
If workers compensation pays for your neck surgery, you may end up with some degree of permanent impairment as a result of your neck injury. Under Georgia law, the workers compensation insurance company should pay you permanent partial disability benefits when you suffer a permanent impairment as a result of a work related injury. These permanent partial disability benefits provide some compensation for the permanent loss of function from your injury.
This article focuses specifically on permanent partial disability benefits for neck injuries under Georgia’s workers compensation law. If you would like to find out more about permanent partial disability benefits (including when the insurance company pays them and when you should receive your permanent partial disability rating), be sure and read this article that covers PPD benefits more generally.
 What should my permanent partial disability rating be for my neck surgery?
What should my permanent partial disability rating be for my neck surgery?
That depends. Georgia law requires doctors to use a certain book to assign your permanent partial disability rating. Currently, Georgia law requirs doctors to use the 5th Edition of the American Medical Association’s Guide to the Evaluation of Permanent Impairment.
This book is over 600 pages. The spine is covered in Chapter 15 of American Medical Association’s Guide to the Evaluation of Permanent Impairment. Most workers compensation neck injuries are rated using Chapter 15.
There are a few different ways that doctors might rate a neck surgery, but the most common method is the Diagnosis-Related Estimates Method. This method is known as DRE for short.
Using this method, permanent partial disability rating for neck injuries fall into one of five different categories. Almost all neck surgeries result in a rating that falls into Category III, IV, or V. Some other types of neck injuries which do not require surgery can fall into Category I or II.
DRE Cervical Category III ratings of 15 to 18 percent to the body as a whole
This is usually the lowest category rating that you see following neck surgery in a Georgia workers compensation case. The part of Category III that talks about surgery says, “individual had clinically significant radiculopathy, verified by an imaging study that demonstrates a herniated disk at the level and on the side expected from objective clinical findings with radiculopathy or with improvement of radiculopathy following surgery.”
So, what does that mean? The definition has three important parts.
The first is radiculopathy. This likely means you had pain, weakness, or numbness radiating from your spine into another area of your body as a result of nerve compression. With cervical injuries, this is often pain that radiates into some part of the arms.
The rest of the definition of this rating is a little more confusing. It discusses an imaging study which verifies a herniated disk that is the likely cause of the radiculopathy. This would typically be an MRI which shows a herniated disk where the doctor would expect it.
In the case of surgery, it also says this rating covers “improvement of radiculopathy following surgery”. If surgery improves or cures the radiculopathy, it is not clear whether you have to have the MRI showing the herniated disk in order to get a Category III rating of 15 to 18 percent to the body as a whole.
DRE Cervical Category IV ratings of 25 to 28 percent to the body as a whole
Cervical fusions are the most common workers compensation neck surgeries that result in Category IV ratings. The language that covers cervical fusions under Category IV is, “… the individual may have loss of motion or a motion segment due to a developmental fusion or successful or unsuccessful attempt at surgical arthrodesis; radiculopathy as defined in cervical category III need not be present if there is alteration of motion segment integrity.”
Surgical arthrodesis refers to cervical fusion. So, a workers compensation injury that requires a cervical fusion surgery should result in at least a Category IV rating of 25 to 28 percent to the body as a whole.
This is the case even if the cervical fusion is completely successful and completely relieves all radiculopathy. The AMA Guides make this clear by giving an example of an individual who has a successful, one level cervical fusion which completely resolves the radiculopathy in the individual’s arms. The example indicates that person would qualify for a Category IV rating of 25 percent to the body as a whole.
It is important to understand this because I have seen many cases where a doctor gives less than a Category IV rating following a cervical fusion. If your workers compensation doctor rated you at Category III following a cervical fusion, your PPD rating would be about 10 percent less than it should have been.
A rating of 10 percent less to the body as a whole is a difference of 30 weeks of permanent partial disability benefits. Depending on the amount of your workers compensation benefits, this could result in you receiving $20,000 or so less than you should have in PPD benefits if you receive $700 a week in PPD benefits.
Fortunately, an incorrect PPD rating can be corrected. But, you or your attorney will have to understand the reason that the rating is incorrect and take steps to get the rating corrected. I discuss this later in this article.
 DRE Cervical Category V ratings of 35 to 38 percent to the body as a whole
DRE Cervical Category V ratings of 35 to 38 percent to the body as a whole
Category V ratings are pretty rare. One situation where a Category V rating comes up is when the neck injury requires an individual to use adaptive devices to compensate for the symptoms from the injury.
The AMA Guides do not fully spell out what they mean by adaptive devices, but they do give a general example. The example indicates that an individual who had a cervical fusion and still has radiculopathy but has to use adaptive devices to grip and turn objects would qualify for a Category V rating.
The question is how significant the adaptive devices needs to be. Would it be enough if you have to use a jar opener or other gripping device because of weakness in your hands and arms or does it require something more significant?
The AMA Guides are not completely clear, so it leaves room to argue that you may qualify for a Category V rating if you continue to have significant impairment in your arms after treatment.
Arguing for a higher rating in this situation would often be worthwhile because there is roughly a 10 percent different between a Category IV and a Category V rating. As I discussed above, these additional weeks of PPD benefits could result in a much higher overall PPD payment.
Are there other ways to assign PPD ratings for neck surgeries?
Yes. There are other methods to assign PPD ratings following neck surgeries. Some of the other methods include Corticospinal Tract Impairment and the Range-of-Motion Method. These methods are seen less frequently than the DRE method.
Corticospinal tract impairment comes up when you have neck surgery to repair a spinal cord injury. This impairment rating method focuses on how your neck injury effects your use of the following body functions:
- Arms
- Legs
- Bowel
- Bladder
- Sexual Function
- Breathing
Spinal cord impairments are serious injuries. The corticospinal tract impairment may be used to rate injuries where an individual had an injury or surgery that would often be rated using the DRE method, but the DRE method does not fully account for their loss of function. With spinal cord injuries, the corticospinal tract impairment method can provide a more accurate method of assessing the loss of function.
The Range-of-Motion method focuses more on combining the particular diagnosis and surgery along with measurements of spinal range of motion. It is used much less frequently than the DRE Method, so I am not going to discuss it in detail here.
 What if I believe the workers compensation doctor may have assigned the incorrect PPD rating?
What if I believe the workers compensation doctor may have assigned the incorrect PPD rating?
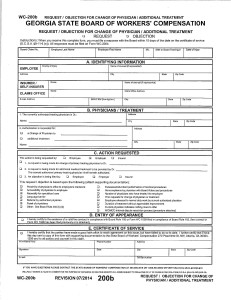
Your workers compensation authorized treating physician usually assigns the PPD rating. The insurance company usually pays PPD benefits based on that rating. So, if your authorized treating physician assigns the wrong rating, you will not receive the benefits you should.
Fortunately, actions can be taken to correct an incorrect PPD rating. Some of the options include:
- Pointing the incorrect rating out to the authorized treating physician and having a revised rating issued
- Getting an opinion from another physician with the correct rating
- Going to court and proving the correct rating to a workers compensation judge
Which one of these actions is best to take will depend on the particular facts of your case. For example, the doctor who issued your rating may not respond very well to being told that you think the rating they issued is wrong. Also, going to court will probably not help if you do not have the evidence to support your argument.
Also, you need to understand that there are deadlines known as statutes of limitations that apply to payment of PPD benefits. This means that waiting too long to get the rating corrected could result in the insurance company not having to pay the correct amount of benefits.
So, be sure that you do not wait if you think your rating is incorrect. It is important to figure out the right strategy and take action to correct the rating.
What other issues will likely come up in my case if I have had neck surgery?
If you have neck surgery in a workers compensation case, these are a few of the issues you could face in the future:
- Will you need ongoing medical treatment for pain and other symptoms after neck surgery? If so, what time limits are there on getting that medical treatment?
- Will your employer continue to provide you with a suitable job?
- Does your injury potentially qualify for a catastrophic designation?


 What if I believe the workers compensation doctor may have assigned the incorrect PPD rating?
What if I believe the workers compensation doctor may have assigned the incorrect PPD rating?